From the Editor
What are the physical side effects of antidepressants? In a new, impressive Lancet study, Toby Pillinger (of King’s College London) and his co-authors attempt to answer that old question with a new approach: the first systematic review and meta-analysis. They drew on 168 RCTs that measured physical health effects of antidepressants, including almost 59 000 participants and comparisons of 30 antidepressants. “We found strong evidence that antidepressants differ markedly in their physiological effects, particularly for cardiometabolic parameters.” We consider the paper and its implications.

How safe is cannabis for those taking it for medical purposes? Dr. Beth Han (of NIMH) and her colleagues report findings from a US survey in a new JAMA Psychiatry brief report, focusing on cannabis use disorder (CUD). They report that cannabis use wasn’t less addictive when used for medical reasons. “Clinicians should consider addiction risk before recommending medical cannabis and, if they do, should monitor for CUD emergence.”
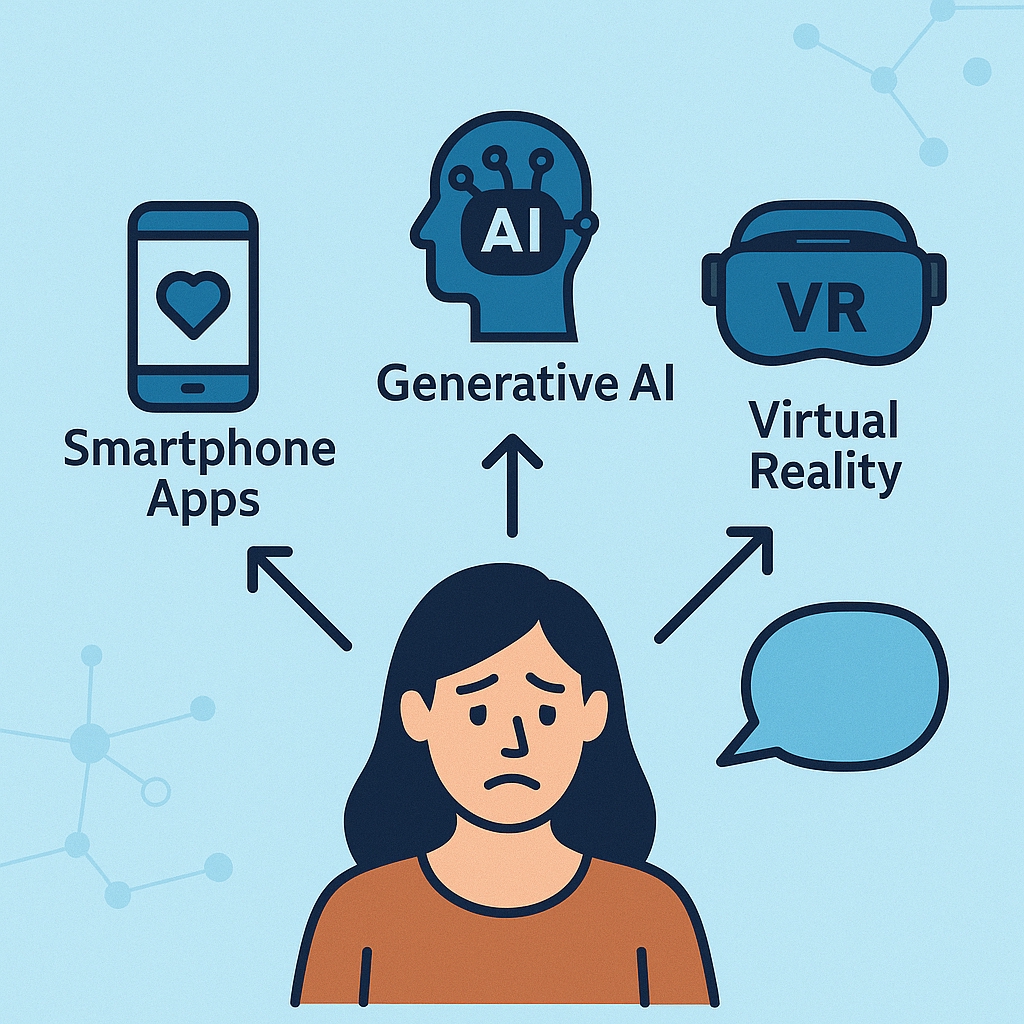
The BMJ runs humorous articles in its Christmas issue. The journal doesn’t disappoint this year. Dr. Roberto A. Correa Soto (of the Universidad de los Andes) and his co-authors write about AI hallucinations and doctor BS (yes, you read that correctly). Frankly, the paper is worth reading for the profanity alone. “Both doctors and large language models (LLMs) are driven to produce misinformation – ‘bullshit’ and ‘hallucinations’ – owing to a shared pressure to provide answers, prioritising the appearance of competence over accuracy.”
There will be no Readings for the next three weeks.
DG





Recent Comments